 What is an Anal Fissure
What is an Anal Fissure
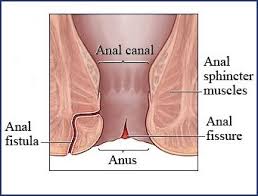
An anal fissure is a small tear in the lining (mucosa) of the anus. Typical symptoms associated with anal fissures are pain and bleeding. Fissures are quite common, but are often confused with other causes of pain and bleeding, such as hemorrhoids.
The pain associated with an anal fissure occurs during or after a bowel movement and may feel like a tearing, burning, or ripping sensation. Once a fissure develops, the painful symptoms may accompany every bowel movement thereafter. The pain may last anywhere from several minutes to hours. Often times patients may try to avoid defecation in fear of experiencing the intense rectal pain.
Bleeding with anal fissures is usually mild and consists of small amounts of spotting on toilet paper or streaking the surface of stool. However, even the slightest amount of blood in the toilet bowl may discolor the toilet water, and give the appearance of heavy bleeding. As the fissure persists, the bleeding may stop, but the pain will generally continue. Some patients also notice itching or irritation of the skin around the anus.
Causes of Anal Fissure
Anal fissures are usually the result of trauma to the inner mucosal lining of the anus. Most commonly this occurs when the anal canal stretches after a hard, dry bowel movement. Other causes of a fissure include diarrhea or inflammatory conditions of the anal area. Less commonly, an anal fissure may result from foreign body insertion or anal intercourse. Once a fissure develops, the internal anal sphincter typically goes into spasm, which causes a decrease in blood flow to the area of the fissure and leads to further separation of the tear, impairing healing and causing pain. Exposure to feces also slows healing. Anal fissures present for less than six weeks are described as acute, while those present for over six weeks are described as chronic fissures. Chronic fissures often have a small external skin tag associated with the tear called a sentinel pile.
Anal Fissure Treatment
The aim of treatment for anal fissures involves relieving the pain and sphincter spasm which will promote healing of the fissure. Often treating one’s constipation or diarrhea can cure a fissure on its own. Therefore, initial management of anal fissures is directed at controlling constipation, softening stools, and reducing anal sphincter spasm. Acute fissures are typically managed with non-operative treatments and roughly 90% will heal without surgery. A high fiber diet, bulking agents (fiber supplements), stool softeners, and plenty of fluids help relieve constipation, promote soft bowel movements, and aid in the healing process. Increased dietary fiber may also help to improve diarrhea. Warm water sitz baths for 10-20 minutes several times each day are soothing and promote relaxation of the anal muscles, which can also help healing. Occasionally, a variety of special medications may be recommended. A chronic fissure may require additional treatment.
There is always the possibility of fissure recurrence, and it is quite common for a healed fissure to recur after a hard bowel movement. Even after the pain and bleeding has disappeared one should maintain good bowel habits and adhere to a high fiber diet or fiber supplement regimen. If the problem returns without an obvious cause, further diagnostic studies may be needed.
 Surgery for Anal Fissures
Surgery for Anal Fissures
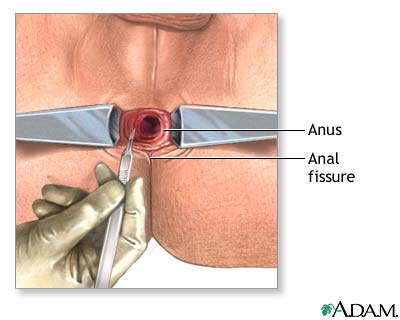
Surgical treatment of anal fissures is generally reserved for those patients who have not healed their fissure after at least three months of medical therapy. Surgical treatment for anal fissures is highly effective and recurrence rates after surgery are low. The procedure usually involves cutting a portion of the internal anal sphincter muscle and is termed a lateral internal sphincterotomy. This helps the fissure heal and decreases pain and spasm. If a sentinel pile is present, it too may be removed to promote healing of the fissure. A sphincterotomy is usually performed as a short outpatient procedure. Fecal incontinence is an extremely rare complication of the procedure. Some patients will experience almost immediate relief of their pain following the procedure. More commonly, the pain disappears after a few days. Patients often return to normal activity within one week. Complete healing occurs in a few weeks.
